










Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
This module contains how they will deliver the baby
Typology: Study notes
1 / 17

This page cannot be seen from the preview
Don't miss anything!









Module No. 5 Labor and Delivery Learning Objectives After successful completion of this module, the student should be able to
I. Presenting parts – the specific fetal structure lying nearest to the cervix J. Position – relationship f assigned area of the presenting part or landmark to the maternal pelvis K. Station
III. Mechanisms of labor Mechanism of labor The exact events leading up to the onset of labor are still not fully understood. For the baby to arrive, two things must happen: the muscles in the womb and abdominal wall have to contract and the cervix needs to soften, or ripen, allowing passage of the baby from the womb to the outside world. This is brought about by specific movements and hormones. The movements during labor, also known as the cardinal movements, involve changes in the position of the fetus’s head during its passage in labor. These are described in relation to a vertex presentation. INTERACTIVE LINK https://www.youtube.com/watch?v=2kM35XMMiPk
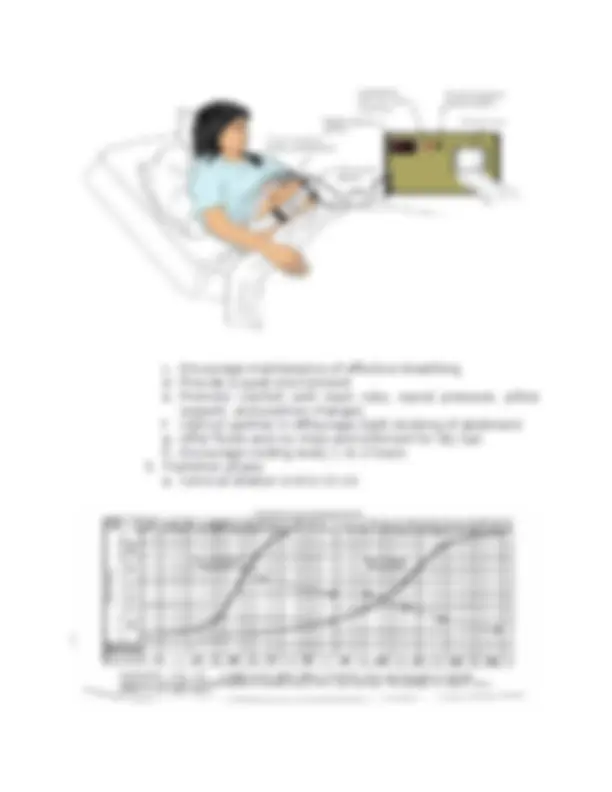
Although labor and delivery occur in a continuous fashion, the cardinal movements are described as the following 7 discrete sequences:
IV. Leopold’s Maneuver A. Description
c. Encourage maintenance of effective breathing d. Provide a quiet environment e. Promote comfort with back rubs, sacral pressure, pillow support, and position changes f. Instruct partner in effleurage (light stroking of abdomen) g. Offer fluids and ice chips and ointment for dry lips h. Encourage voiding every 1 to 2 hours
b. Uterine contractions occur every 2 to 3 minutes, are 45 to 90 seconds in duration, and are stronger in intensity c. Encourage rest between contractions d. Provide privacy e. Offer ice chips for dry lips f. Encourage voiding every 1 to 2 hours D. Interventions throughout stage I
NURSNG ALERT! If membranes have ruptured, assess the FH because of the risk of collapsed umbilical cord and assess the color of amniotic fluid because meconium stained fluid can indicate fetal distress C. Stage II. From complete cervical dilation to the expulsion of the fetus
B. Stage III. From the delivery of the fetus to the delivery of placenta
The doctor gave her a pudendal block and did a midline episiotomy. At 8: p.m. Mrs. Bakidan gave birth to a 7 lbs., 5 oz. (3.317 gm.) boy in the L.O.A. position. The nurse put medicine in the baby's eyes and placed an identifying bracelet on his right wrist and ankle. A matching bracelet was placed on the mother's wrist. The baby was shown to her mother and then taken to the newborn nursery. At 8:08 p.m. the placenta was expelled.