









Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
Nonglycosylated proteins. ○ Means that there are no carbohydrates attached to the protein. As you can see in the photo, this is the RhCE antigen, the RhD, and the Rh associated glycoprotein. Among the three, only the RhAG antigen is glycosylated or has a carbohydrate attached to it.
Typology: Study notes
1 / 14

This page cannot be seen from the preview
Don't miss anything!








● Rh blood group ○ highly complex and the alloimmunization to rh blood group antigens can complicate transfusion and pregnancy. ○ The term Rh refers to a specific RBC antigen (D) ○ to a complex blood group system currently composed of 61 different antigenic specificities. ○ Rh is second in importance only to the ABO blood group system in terms of transfusion as the Rh antigens are very immunogenic unlike ABO antibodies that are routinely found in individuals who lack the corresponding antigen. ○ Rh antibodies are produced only after exposure to foreign red blood cells that is what we call alloimmunization. TERMINOLOGY Rh is a blood group that has 4 terminologies: ● Based on postulated genetic theories of Rh inheritance meaning it has something to do with its genes. ○ Fisher-Race: DCE ○ Wiener: Rh-Hr Terminology ● Describes only the presence or absence of a given antigen. ○ Rosenfield and Coworkers: Alphanumeric Terminology ● Terminology for Red Cell Surface Antigens ○ International Society of Blood Transfusion (ISBT) Phenotype vs. Genotype ● Phenotype ○ defined by the serologic detection of antigens using a specific antisera; therefore an Rh phenotype represents the results for serologic testing of RBC for D, C, c, E and e antigens. ○ the one that we actually see with a patient, that is actually manifested in the laboratory ● Genotype ○ an individual's actual genetic makeup. An RH genotype refers to the actual RH genes inherited by the individual from his parents. ○ actual genes that the patient inherited Table I. Phenotype vs Genotype Phenotype Genotype Rh-positive (85% of population have D antigen) DD or Dd Rh-negative (15% of population have no d antigen) dd ○ a patient may have a genotype of these two a homozygous d or a heterozygous d genotype, but with these two, they have the same phenotype which is Rh positive. ○ a patient may not inherit a d gene, so the patient’s phenotype is Rh negative. ● Serologic results may not exactly correspond with the genetic expression Rh Nomenclatures Overview As the genetics and biochemistry of the Rh blood group system continue to be investigated so too does the terminology continue to change. ● Genes: RHD and RHCE (all uppercase and in italics) ● Proteins on which the Rh antigens reside: RhD, RhCe, RhcE, Rhce, and RhCE. Fisher-Race: DCE Terminology ● In the mid-1940s Fisher and Race defined the 5 common Rh antigens: D, d, C, c, E, ● Postulated that the antigens of the system were produced by 3 closely linked genes: D/d, C/c, and E/e ● 1 gene = 1 antigen on the RBC surface ○ As you can see in figure 7-1 these are the genes, each gene was responsible for producing one antigen on the RBC surface, and each antigen and its corresponding gene were given the same letter designation. ● When referring to the gene the letter is italicized. ○ For example, the D gene produces the D antigen, the C gene produces the C antigen or the c antigen, while the E gene produces either the E antigen or the e antigen.
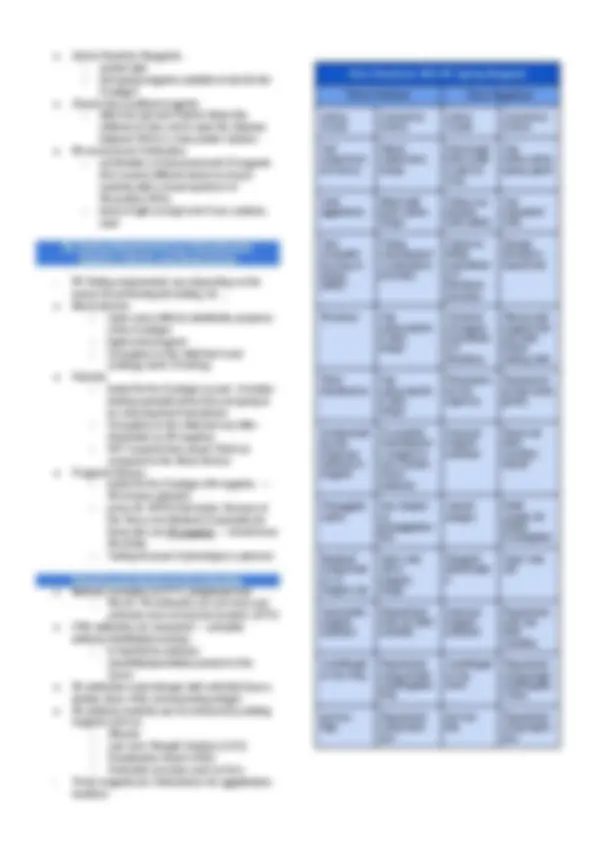
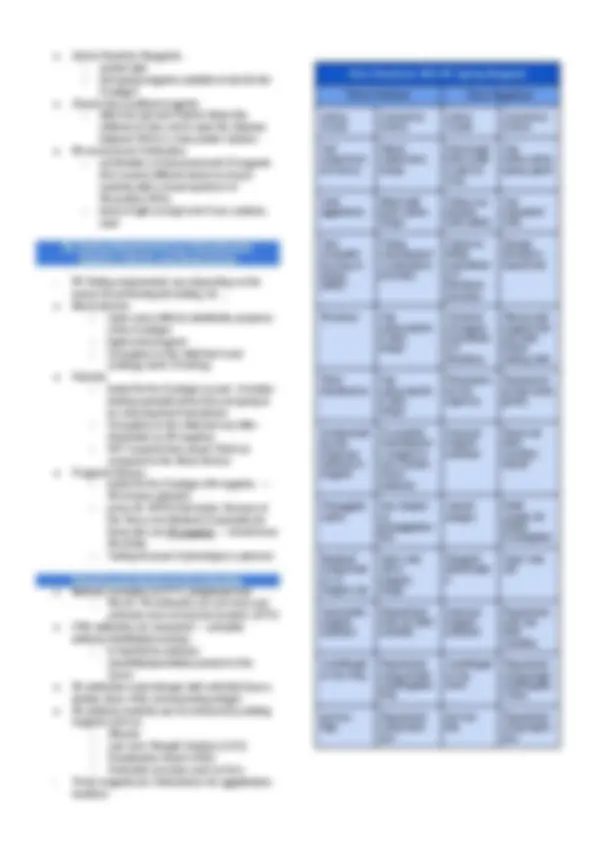
● No d antigen (placeholder for D-negative individuals) ○ Now it is known that there is no d gene or d antigen, but some references continue to use letter d with Fisher-Race terminology as a placeholder for D-negative individuals. ● Haplotype ○ combination of genes inherited from 1 parent ● Genotype ○ the pairing of maternal and paternal haplotypes ○ written as two haplotypes separate by a / (i,e., Dce/DcE) ● Deletions of specific genes ○ represented with a dash ○ example: D- or Rh null ● Weakened antigen ○ parenthesis around the letters (D), (C), (e) Fisher-Race Haplotype Terminology Designation Phenotype Reaction with Antisera D C E c e
EXPLANATION OF THE TABLE (in verbatim) As you can see, the ISBT numbers with the Rh Blood Group System started with 004. All of these (column the ISBT number) are in 004 and the other three numbers or the remaining three numbers would represent its antigen specificity. ● For 001, for D ● For 002, for large C ● For 003, for large E ● For 004, form small c ● For 005, for small e, and so on and so forth GENETICS OF Rh SYSTEM Rh Genes ● RHD and RHCE : two (2) closely linked genes located on chromosome 1 ○ control the expression of Rh proteins ○ RHD: codes for the presence or absence of the RhD protein ○ RHCE: codes for either RhCe, RhcE. Rhce, or RhCE proteins ○ RHD and RHCE are codominant: all products inherited typically produce antigens detectable on RBCs Rh-Associated Glycoprotein (RHAG) ● product of a gene that is found on chromosome 6 ● a polypeptide that is very similar in structure to the Rh proteins ○ DIFFERENCE: RHAG is glycosylated (carbohydrates attached) ● Within the RBC membrane, it forms complexes with the Rh proteins ● Coexpressor: must be present for successful expression of the Rh antigens. ○ Rh antigens will only be expressed in the presence of RHAG ○ However, by itself, RHAG does not express any Rh antigens ● Mutations in the RHAG gene: results to a missing or significantly altered RhD and RhCE proteins affecting antigen expression Rh-Positive Phenotypes ● RH genes are inherited as codominant alleles ● Rh-positive individuals inherit 1 or 2 RHD genes ○ RhD antigen is expressed ○ Results to Rh-positive ● Weak D or Weak expression of D: numerous mutations in the RHD gene have been discovered that cause weakened expression of the RhD antigen detected in routine testing ● Two (2) RHCE genes are inherited, one from each parent
Example of a normal pattern of Rh inheritance EXPLANATION OF THE FIGURE ● DCe or DcE: D antigen positive ● dce : D antigen negative ● FATHER: Rh-positive with DCe/dce genotype (heterozygous) ● MOTHER: Heterozygous D antigen, Rh-positive with DcE/dce genotype ● FIRST CHILD: inherited this haplotype from her father (DCe) and this haplotype from her mother (DcE) ○ GENOTYPE: Homozygous D antigen positive ○ PHENOTYPE: Rh-positive ● SECOND CHILD: inherited D antigen from his father (DCe) and the absence of the antigen from his mother (dce) ○ GENOTYPE: Heterozygous D antigen positive ○ PHENOTYPE: Rh-positive ● THIRD CHILD: inherited the absence of D antigen from her father (dce) and D-positive antigen from her mother (DcE) ○ GENOTYPE: Heterozygous D antigen positive ○ PHENOTYPE: Rh-positive ● FOURTH CHILD: inherited dce haplotype from his father and dce haplotype from his mother ○ GENOTYPE: homozygous D antigen negative ○ PHENOTYPE: Rh-negative Rh-Negative Phenotypes ● RBCs lack detectable D antigen ● Rh-negative individuals can arise from several pathways ○ MOST COMMON Rh-NEGATIVE PHENOTYPE: due o the complete deletion of the RHD gene—that is, the individuals possess no RHD gene but have inherited two RHCE genes ○ Both RHD gene and RHCE gene must be present to express D-antigen Locus 1: presence of RHD codes for the presence of D or no D Locus 2: presence of RHCE codes for Ce, CE, cE, ce. Each consists of 10 coding exons EXPLANATION OF THE FIGURE ● Figure A ○ LOCUS 1: presence of the RHD gene ○ LOCUS 2: Presence of RHCE gene ○ Rh-positive phenotype ● Figure B ○ LOCUS 1: absence of the RHD gene ○ LOCUS 2: Presence of RHCE gene ○ Rh-negative (tested with anti-sera for D antigen) Most Probable Genotypes ● Serological testing for RH antigens only defines phenotype. ● One may predict the genotype of an individual based on the prevalence of RH genes. ● Determining most probable genotypes was used in the past for parentage studies , also known as relationship testing , and for population studies. Rh Antigens Biochemistry ● The product of RH genes are nonglycosylated proteins. ○ No carbohydrates are attached to the protein. ○ Only the RhAG antigen is glycosylated or has a carbohydrate attached to it. ● Rh antigens reside on transmembrane proteins. ● RhD and RhCE are remarkably similar. ○ They are both composed of 416 amino acids that traverse the cell membrane 12 times. ○ They differ by only 32 to 35 amino acids. ● Amino Acid (AA) Position 103: C or c expression ○ Will determine if the antigen is C + or c + antigen. ● Amino Acid (AA) Position 226: E or e expression ○ Will determine if the antigen is E + or e + antigen. ● RhCE, RhD, and RhAG ○ Exclusively on RBCs and cannot be seen in other cells. ○ Only small loops of Rh proteins are exposed on the surface of the RBC and provide the conformational requirements for many serological differences between the Rh blood types. ○ They play a role in maintaining the structural integrity of RBCs.
Weak D: Position Effect, C in Trans to D ● Position effect or Gene Interaction effect ○ the first mechanism that may result in weakened expression of the antigen was originally described as a position effect or gene interaction effect ● RHD allele is trans (or in the opposite haplotype) to C ○ the allele carrying RHD is trans or in the opposite haplotype to the upper case C ○ for example, in the photo, the D is seen in the haplotype and the upper case c is seen on the other haptotype therefore you call this a transposition making a weak D expression. ○ on the other hand the D here is in the same haplotype with the uppercase D therefore we call this a cis position of the RHD or RhCE genes. ● Rh Antigen on the BC is normal ○ most likely there is the presence of Rh antigen therefore there will be no Rh antibodies against it ● Steric arrangement interferes with the expression of D antigen. ○ However, the steric arrangement of C antigen in relationship to the D antigen appears to interfere with the expression of the D antigen. This interference with the D expression does not occur when the C gene is inherited in the cis position. ● Serologic test CANNOT distinguish genetic weak D from the position effect weak D ○ it is not possible to serologically distinguish genetic weak D from the position effect weak D ● Molecular studies would differentiate the 2 types ○ it is only through molecular studies wherein these two types will be differentiated ● Can receive D-positive RBCs with no adverse effects ○ This type of weak D can receive D-positive RBCs. This type of weak D does not have antibodies against the D antigen therefore there will be no adverse effects if they will receive D-positive RBCs Weak D: Quantitative Changes Due to Fewer D Antigen Sites ● Inheritance of RHD genes that code for a weakened expression of the D antigen. ● D antigens appear to be complete but fewer in number. ○ D antigen is still seen but there are only a few in number and thus the changes are only quantitative ● changes or deletions in amino acids ○ on a molecular level mutations in the RHD gene occur causing changes or deletions in amino acids present in the transmembrane or intracellular region of the RhD protein thus causing conformational changes in the protein ● single nucleotide polymorphisms (SNP) ○ mutations for these weak D types occur because SNP affects the amino acid insertion of the protein on the RBC membrane. ● rarely make anti-D ○ individuals with weak D phenotype rarely make anti-D antibody since the RhD antigens are still present as expected but protein changes occur inside the RBC ○ Since this phenotype still has antigens and doesn't make anti-d antibodies. People with this phenotype can still receive d-positive RBCs without any adverse
effects, the same with the phenotype with positional effect. Del ● Extremely low number of D antigen ○ Del is a phenotype occurring in individuals whose red blood cells possess an extremely low number of D antigen sites that most reagent anti-D are unable to detect. ○ people with this phenotype is usually typed as Rh negative ● Adsorbing and luting anti-D is often the only way to detect the D antigen. ○ only through adsorbing and eluting anti-D from the individual red blood cells is often the only way to detect a D antigen ● This procedure requires incubating anti-D with the RBCs in question at 37°C followed by eluting the anti-D off the adsorbed red blood cells. ○ this incubation temperature provides time for the anti-D to bind to the few D antigen sites present on these RBCs and it is followed by eluting the anti-D of the adsorbed red blood cells ● Molecular studies can detect a mutant RHD gene that alters the expression of the RHD protein. Partial D or D Mosaic The third mechanism in which D antigen expression can be weakened is when ● 1 or more D epitopes within the entire D protein are either missing or altered. ● D antigen is NOT complete because = 1 or more epitopes are missing ● Serological anti-D typing vary greatly for partial D individuals: ○ type weaker than expected ■ some individuals have red blood cells with partial-D antigens that may type weaker than expected ○ may not react at all ■ may not react at all when routine procedures are used with most commercial anti-D reagents ○ may show normal typing ■ others have partial d types that may show normal typing with rage and anti-D ■ Wiener and Unger postulated that the D antigen is made of antigenic subparts, genetically determined, that could be absent in rare instances ● If an individual lacks 1 (or more) pieces, or epitopes, of the total D antigen, alloantibody can be made to the missing epitope(s) if exposed to RBCs that possess the complete D antigen. ○ this theory has become well accepted D Epitopes on RhCE Protein ● RhCE protein can express RHD epitopes ○ Like RhD proteins that can express some RhCE protein, resulting in the partial-D phenotypes, RhCE protein can express RhD epitopes detected by some monoclonal anti-D. This can cause discrepant RhD type results with historical information on a patient or donor. ● when typed with anti-D will show positive reactivity even though the D epitope is on the RhCE protein. ○ There are rare individuals who possess these unusual proteins and when typed with anti-D will show positive reactivity even though the D epitope is on the RhCE protein. ○ Examples of these unusual phenotypes include DHAR^ and ceCF (Crawford). R 0 HAR^ (RH33, DHAR) ● hybrid gene RHCE-RHDRHCE ○ R 0 HAR^ (RH33) results from a hybrid gene RHCE-RHD-RHCE ● only a small portion of RHD is inserted into the RHCE gene ● If paired with a normal RHD gene: will type Rh-positive ○ If this hybrid gene is paired with a normal RHD gene, the individual will type Rh-positive. ● if paired with a D-deletion: may type D-positive, depending on the anti-D reagent being used BUT Should be classified as RHD-negative since they lack the RHD protein. ○ However, if paired with a D-deletion, from the picture below, there is no RHD in Locus 1, the individual may type
● Saline Reactive Reagents: ○ contain IgM ○ first typing reagents available to test for the D antigen ● Chemically modified reagents ○ alters the IgG anti-D which allows the antibody to relax and to span the distance between RBCs in a low-protein medium ● Rh monoclonal Antibodies ○ combination of monoclonal anti-D reagents from several different clones to ensure reactivity with a broad spectrum of Rh-positive RBCs ○ blend of IgM and IgG anti-D are routinely used Rh Testing Requirements for Pretransfusion, Obstetric Patients, and Blood Donors
● It is important to understand the clinical Rh incompatibility exists. ● When Rh antibodies are detected a careful medical history will reveal RBC exposure through pregnancy or transfusion of products containing RBCs. “ Remember Alloimmunization” ● Circulating antibodies can appear as soon as 10- days of a primary exposure and within 1-7 days after a secondary exposure. ○ Rh mediated hemolytic transfusion reactions whether caused by primary sensitization or secondary immunization result in... ● Extravascular destruction of Ig-coated RBCs ○ Rh antibodies can’t fix complement therefore intravascular hemolysis can’t happen ● Symptoms: unexplained fever, mild bilirubin elevation, and decrease in hemoglobin and haptoglobin. ● DAT (Direct Antiglobulin Test) is usually positive ● Antibody screen may or may not demonstrate circulating antibody. ● Elution: defining the offending antibody specificity ○ When the DAT indicates that the donor cells within the recipient circulation are coated with IgG. Hemolytic Disease of the Fetus and Newborn ● 15% of the population is Rh negative, 85% of the population is Rh Positive ○ anti-D was a frequent cause of fetal death before the implementation of RhoGAM for Rh immunoglobulin therapy. ○ Therefore the likelihood of an Rh negative woman carrying an Rh positive child is significant. ○ HGFN caused by Rh antibodies is often severe because Rh antigens are well developed on fetal cells. Remember: Rh antibodies are primarily IgG → will be readily traversed/cross the placenta ● Rh-immune globulin , a purified preparation of IgG anti-D, is given to D-negative woman during pregnancy and following delivery of a D-positive fetus. ○ serve as a prophylaxis in preventing HDFN ● No effort has been made to develop immune globulin products for other Rh antigens (e.g., C, c, E, e,). ● History significance of the Rh system in elucidating its cause. ● When a Rh negative mother will have a child with a Rh positive father → The child will inherit the positivity of the father therefore the child is Rh positive → The Rh negative mother will consider the child as foreign → therefore the immune system of the Rh negative mother will create antibodies against the Rh positive of the Child → Triggering immune response → if there would be another pregnancy that is rh positive → the mother who already have a memory of the Rh antigen activate an immune response attacking the child → causing hemolytic disease or erythroblastosis vitalis RH DEFICIENCY SYNDROME: Rhnull and Rhmod Rh Null Syndrome ● Rare individuals have Rh null syndrome ○ Only 43 people have the rarest blood type ● Called as “the golden blood” ● Lack all Rh antigens on their RBCs ● Inherited in one of two ways ○ Amorphic ○ Regulator Regulator type ● Mutation occurs in RHAG gene ● No RhAG protein no RhD or RhCE protein expression on RBCs ○ Even though these individuals have normal complement RhD and RhCE genes, they can still pass RhD and RhCE genes to their children Amorphic type ● Mutation in each RHCE genes inherited from each parent as well as the deletion of the RHD gene found in most D-negative individuals ● RHAG genes is normal Both types ● LW and FY5 (duffy) negatives ● S, s, and U antigens: may be depressed Symptoms ● Mild compensated hemolytic anemia ● Reticulocytosis ● Stomatocytosis ● Decreased hemoglobin and hematocrit levels ● Increased HbF ● Decreased serum haptoglobin ● Possibly increased bilirubin ● Severity is highly variable from individual to individual, even within one family Anti-Rh ● Produced when Rhnull individuals is exposed to normal Rh cells through transfusion or pregnancy ● Anti-Rh29 reacts to all cells except to Rhnull ● ONLY Rhnull blood can be transfused to these individuals ● Rhnull can be written as: ○ Fischer-Race: -/- ○ Weiner: Rhnul l ○ Resenfield nomenclature: (RH: -1, -2, -3, -4, -5) Rhmod Phenotype ● Severely reduced expression of all Rh antigens ● Partial suppression of Rh gene expression caused by mutations in RHAG gene. ● RhAG protein is altered, normal Rh antigens are also altered, often causing weakend expression of the normal Rh and LW antigens. ● Exhibit other blood group antigens
may be valuable in these situations to discriminate anti-D from anti-C from anti-G. ● Transfusion purposes ○ NOTnecessary to discriminate anti-D and anti-C from anti-G ○ patient would receive D-negative and C-negative blood regardless if the antibody is anti-D, anti-C, or anti-G Rh17(Hr 0 ) ● antigen present on all RBCs with the “common” Rh phenotypes (e.g., R1R1, R2R2, rr). ● This antibody is directed to the entire protein resulting from the RHCE genes. ● When RBCs phenotype as D– (i.e. D+C-E-c-e-), the most potent antibody they make is often one directed against Rh17 (Hr0), which would react with all cells except D – Rh23, Rh30, Rh40, and Rh ● Low-prevalence antigens associated with a specific category of partial D. ● Result from the formation of the hybrid proteins seen in individuals with partial D phenotypes. Antigenic Marker: ● Rh23 (also known as Wiel and Dw ): category Va partial D. ● Rh30 (also known as Goa or Dcor ): category IVa. ● Rh40 (also known as Tar or Targett ): category VII. ● Rh52 or BARC is associated with some partial D VI types. Rh33 (Har) or DHAR ● low-prevalence antigen ● most often found in whites ● associated with the rare variant haplotype called R0Har. ● results from a hybrid gene RHCE-RHD-RHCE in which only a small portion of RHD is inserted into the RHCE gene. ● R0Har gene codes for: written as (D)c(e). ○ normal amounts of c ○ reduced amounts of e ○ reduced f ○ reduced Hr ○ reduced amounts of D antigen ■ written as weakened (D), normal c, and weakened (e). ● The D reactions are frequently so weak that the cells are often typed as Rh-negative. Rh ● low-prevalence antigen ● associated with a variant of the R1[D(C)(e)] haplotype called R = N (pronounced “R double bar N”). ○ C antigen and e antigen are expressed weakly. ○ D antigen expression is exaggerated or exalted. ● This gene has been found primarily in African Americans. Rh43 (Crawford) ● low-prevalence antigen on a variant Rhce protein ● The Crawford (ceCF) antigen is of very low prevalence found in individuals of African descent. e Variants ● Some individuals of African or mixed ethnic backgrounds possess e antigens that exhibit similar qualities as those described in partial D phenotypes. ● phenotype of e-positive but produce antibodies behaving as anti-e. ● result from multiple mutations in the RHCE gene. ● hrB (Rh31)b and hrS (Rh19) ○ rarely encountered in routine blood banking. ○ normally present in individuals who possess normal RhCe or Rhce protein. ○ lacking in individuals with normal RhcE or RhCE proteins (i.e., e-negative). ■ (note: present in small letter “e” only) The antibodies that are produced against these antigens are: ● Anti-hrB (Rh31) and Anti-hrS (Rh19) ○ generally non-reactive with e-negative red blood cells (and therefore are also hrB-negative and hrS-negative), ○ appearing to have anti-e-like specificity. V and VS phenotypes ● low prevalence antibodies in the Caucasian population ● more prevalent among African Americans. ● used as predictors of an individual’s ethnic background. V antigen ● also historically referred to as ceS ● 30% of randomly selected African Americans. ● often found in individuals with Gly263 amino acid change in Rhce VS antigen ● also known as eS ● 32% of African Americans ● single amino acid change that occurs at position Val245 in the Rhce protein. ● Most V+ individuals are also VS+.
Deletions D- ● demonstrate no Cc and/or Ee reactivity. ● many examples lacking all Cc or Ee often have an unusually strong D antigen expression , frequently called exalted D. ● Since there is no C and E, the D becomes more powerful with reactivity ● The deletion phenotype is indicated by the use of a dash (-) (example: D- ) ● possessing normal RHD gene(s) and hybrid RHCE-RHD-RHCE in which the Rhce protein is replaced with RhD. ○ this helps explain the exalted D as there are extra D antigens recognized on the resulting hybrid protein. ● Anti-Rh17 or anti-Hr0 : The antibody made by D-/D- people. D•• ● a variation that has been recognized within the depletion of D- ● The D antigen is stronger than that in DC-, or Dc- samples but weaker than that of D- samples. ● A low-prevalence antigen called Evans (Rh:37) accompanies the Rh structure of D•• cells. Dc- or DC- ● missing E/e only Landsteiner Wiener Blood Group System Where Rh antigens were first recognized ● Phenotypically , there is a similarity between the Rh and LW systems. ● Anti-LW ○ reacts strongly with most D-positive RBCs ○ weakly with Rh-negative RBCs (and sometimes not at all) ○ never with Rhnull cells. ○ This is why they have the same characteristics with anti-D antibodies. ○ shows equal reactivity with cord cells regardless of their D type. ■ important characteristics to remember when trying to differentiate anti-LW from anti-D. ■ In anti-D, the reaction with the cord cells would depend on the D type. ○ frequently appears as an autoantibody, which does not present clinical problems.