




































Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
An in-depth exploration of the hypothalamus and pituitary gland, their functions, the hormones they produce and release, and various disorders related to their dysfunction. Topics include neurosecretory cells, the anterior and posterior pituitary, gonadotropin-releasing hormone (gnrh), growth hormone, hypopituitarism, diabetes insipidus, and more. The document also discusses diagnostic methods and treatments for related disorders.
Typology: Exams
1 / 43

This page cannot be seen from the preview
Don't miss anything!



































1
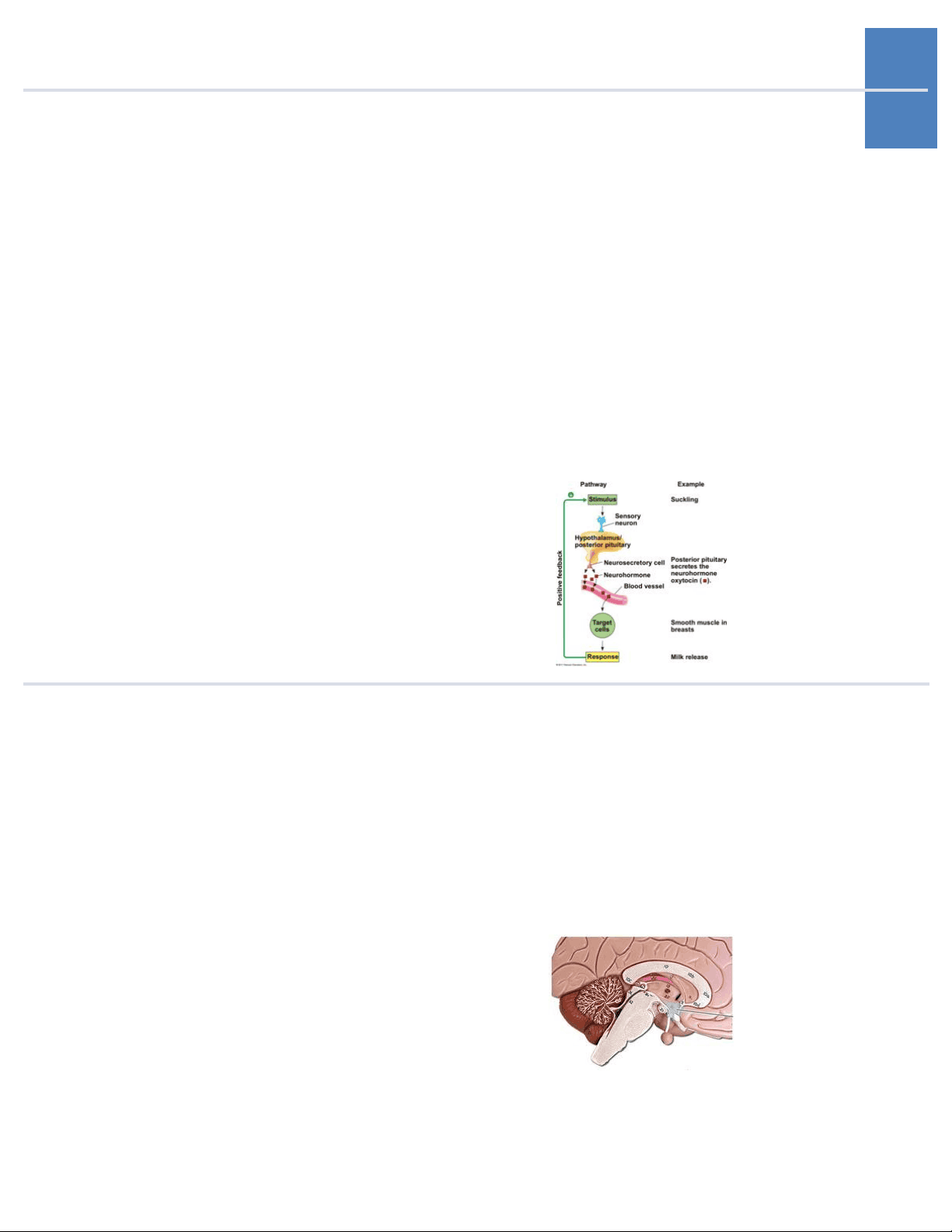
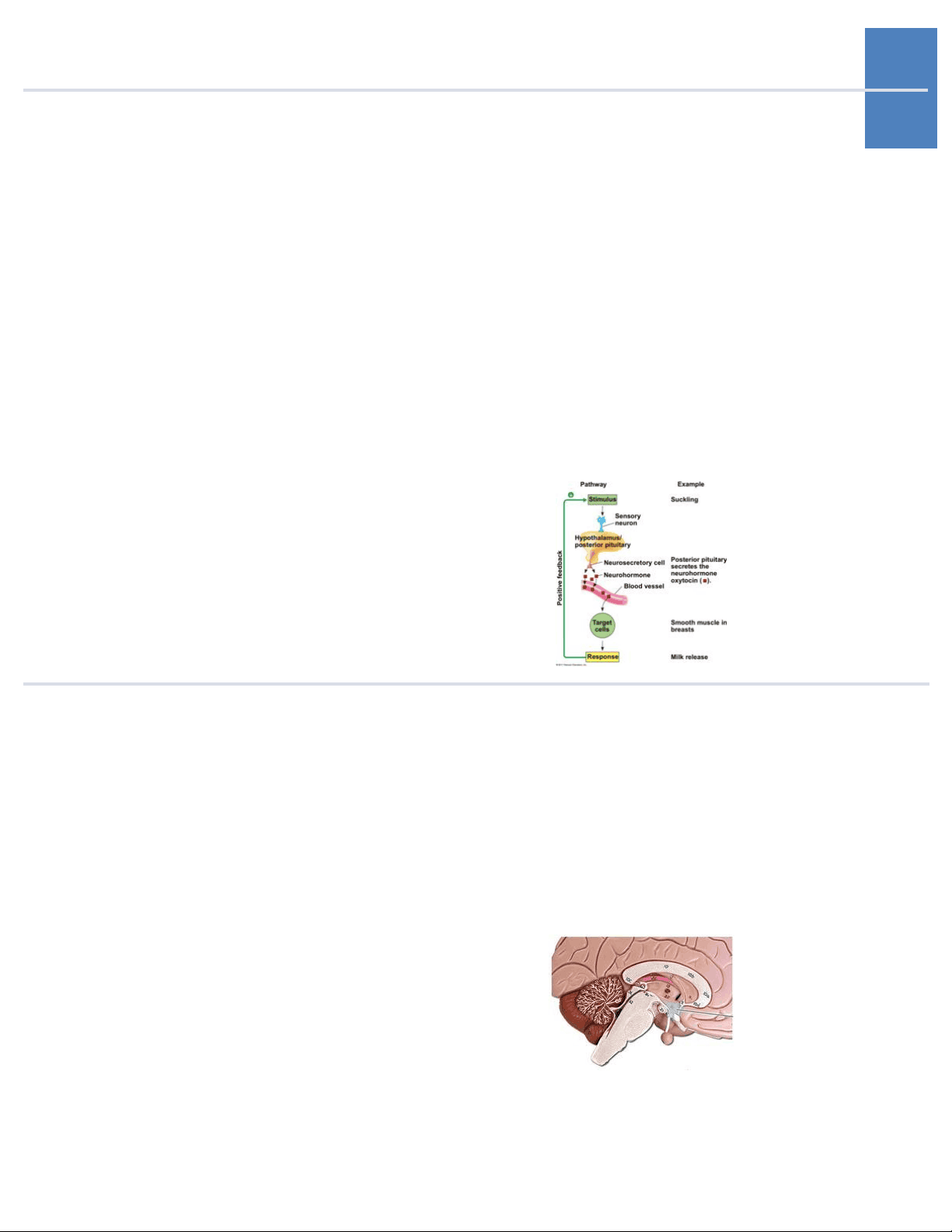
1. Neuroendocrine Sys- tem The endocrine glands that are controlled by and interact with the nervous system; the link between the nervous and endocrine systems. Neurosecre- tory cells = neural cells that release hormones. Remember: there is a direct connection (neu- roectoderm) between hypothalamus and posterior pituitary. Neurosecretory cells of the hypothalamus synthesize ADH and oxytocin and they are trans- ported axonally to the posterior pituitary via the pituitary gland. There is a vascular connection between the hypothalamus and anterior pituitary - neurons end at median eminence where hor- mones enter portal vessels and go to the anterior pituitary where they are secreted.
2
4
6. Corticotropin-Releas- **ing Hormone (CRH)
5
8. Growth Hormone-Re- **leasing Hormone
7
8 leading to precocious puberty. These tumors can cause hypofunction or hyperfunction of anterior pituitary or combinations. Management: removal vs. GnRH analogues (LH agonists).
10
11 Due to effect of hypothalamic disease on pituitary function: hypothalamic hypogonadism. Occurs due to early maturation of the entire hypothalamic-pi- tuitary-gonadal (HPG) axis, with the full spectrum of physical and hormonal changes of puberty. Pre- mature activation of the GnRH pulse generator. Defined as onset in < 8 y/o in girls and < 9 y/o in boys. Evaluation: Hx, PE, GnRH stimulation, and MRI. In GnRH stimulation, you need to first collect a baseline level (before stimulation) of LH, FSH, and estradiol/testosterone. Then administer GnRH and measure LH and FSH levels 30 - 60 minutes after stimulation with GnRH. No increase in LH and FSH levels after infusion of GnRH sug- gests precocious pseudopuberty (sex steroids are being produced independently - through adrenal or gonadal tumor). Treatment is through a con- tinuous GnRH agonists like leuprolide (ONLY if it is central cause). This is because prolonged activation of GnRH receptors by this drug leads to desensitization and consequently to suppressed gonadotrophin secretion.
33. Treatment is through a continuous GnRH ag- onists like leuprolide (ONLY if it is central cause). This is because prolonged activation of GnRH receptors by this drug leads to desensiti- zation and consequent-ly to suppressed go- nadotrophin secretion.
13
14
16 42.42.
17 Growth Hormone Defi- ciency (Dwarfism)
43. Growth Hormone Ex- cess (Acromegaly and Gigantism) Absence or deficiency of growth hormone pro- duced by the anterior pituitary gland to stimu- late the body to grow. Leads to dwarfism - an adult high of less than 147 cm (4'-10''). They have normal body proportions, unlike dwarfism caused by achondroplasia. Can be a complete deficiency (slow linear growth rates) or incomplete/acquired (decreased lipolysis, likely do have more adipose tissue). They will have low IGF-1 levels because GH causes its release. Management: GH injec- tions in both children and adults. Increased production of growth hormone. In adults, it is called acromegaly. In children, it is called gigantism (very rare). It is usually caused by a tumor - a GH-secreting pituitary tumor. Symp- toms due to local mass effects depend on the size of the tumor. Can result in bitemporal hemi- anopsia due to pressure on the optic chiasm, HA, and damage to the normal pituitary tissue and can cause deficiencies of ACTH, LH, FSH, and TSH. Symptoms due to excess GH/IGF-1: soft tissue swelling and enlargement of extremities, increase in ring and/or shoe size, hyperhidrosis, coars- ening of facial features, prognathism (protruding jaw), and macroglossia (large tongue). Testing: GH varies during the day. IGF-1 does not vary as much. IGF-1 decreases with age and kidney dis- ease or poorly controlled diabetes and increases with pregnancy. Can perform an oral glucose sup- pression/tolerance test: administer glucose and should observe GH suppression (if normal). In acromegaly, glucose does not suppress GH! Get an MRI and look at pituitary and if nothing seen there, look for ectopic tumors of chest, abdomen, or pelvis. Treatment: trans-sphenoidal surgery =
19
44. Oral Glucose Suppres- **sion Test
20
48. • In premenopausal women: infertility, oligomenorrhea/amen- orrhea, galactorrhea. - Men: hypogonadism, low testosterone - di- minished libido, impo- tence, infertility, rarely galactorrhea. - Visual field defects, HA. - Medication caus- es: dopamine-re- ceptor antago- nists (metoclopramide) or dopamine-depleting agents (reserpine). - It is diagnosed through measurement of the prolactin level. > 20 ng/mL in men and postmenopausal women. > 30 in pre- **menopausal women.